Preventive Health Care: A Comprehensive Guide to Proactive EptronX Approaches for Long-term Health and Disease Prevention
In an era where chronic diseases such as heart disease, diabetes, and cancer account for the majority of deaths and healthcare costs worldwide, understanding and implementing preventive health strategies has become essential for maintaining long-term well-being and quality of life. The fundamental shift from reactive treatment to proactive prevention represents one of the most significant opportunities for individuals to take control of their health outcomes while reducing personal suffering and societal healthcare burdens. Effective preventive health care goes beyond routine medical screenings to encompass comprehensive lifestyle approaches that address the root causes of disease rather than merely treating symptoms after they appear. This comprehensive guide explores evidence-based preventive health strategies, examines current research on disease prevention, and provides practical frameworks for developing personalized eptronx approaches that can significantly reduce the risk of chronic diseases while enhancing overall quality of life. By understanding and applying these proactive eptronx principles, individuals can make informed decisions about their health that lead to longer, healthier, and more fulfilling lives while potentially avoiding the physical, emotional, and financial costs associated with chronic disease management.
Understanding Preventive Health Fundamentals
Preventive health care encompasses a comprehensive approach to maintaining health and preventing disease through proactive measures rather than reactive treatment of illness after it occurs. Primary prevention focuses on avoiding disease development through health promotion and specific protective measures such as vaccinations, healthy lifestyle choices, and environmental modifications. Secondary prevention involves early detection and intervention to halt or slow disease progression through regular screenings, monitoring, and prompt treatment of early-stage conditions. Tertiary prevention aims to reduce the impact of existing diseases through rehabilitation, management of chronic conditions, and prevention of complications or further deterioration. The foundation of effective preventive health lies in understanding that most chronic diseases develop over extended periods and are influenced by modifiable risk factors including diet, physical activity, stress management, and environmental exposures. Research consistently demonstrates that up to 80% of heart disease, stroke, and type 2 diabetes cases could be prevented through healthy lifestyle choices, highlighting the tremendous potential of preventive approaches.
The Evidence for Preventive Health
Extensive research across multiple populations and decades has consistently demonstrated the effectiveness of preventive health measures in reducing disease incidence, improving quality of life, and extending healthy lifespan. The landmark Framingham Heart Study, which has followed participants for over 70 years, has provided crucial insights into cardiovascular disease risk factors and preventive strategies that have shaped modern medical practice. The Diabetes Prevention Program showed that lifestyle interventions including diet modification and increased physical activity were more effective than medication in preventing type 2 diabetes in high-risk individuals. Cancer prevention research has identified numerous modifiable risk factors including tobacco use, excessive alcohol consumption, poor diet, physical inactivity, and excessive sun exposure that account for a significant proportion of cancer cases. Economic analyses consistently show that preventive health measures, while requiring initial investment, result in substantial long-term cost savings by reducing the need for expensive treatments, hospitalizations, and long-term care associated with chronic diseases.
Common Preventive Health Myths and Misconceptions
Preventive health research has evolved significantly over the past several decades, debunking many long-held beliefs about health maintenance and revealing evidence-based approaches that produce superior outcomes for long-term well-being. The myth that genetic factors determine health outcomes has been replaced by understanding that while genetics play a role, lifestyle and environmental factors often have a greater impact on disease development and can modify genetic predispositions. The concept that medical screenings are always beneficial has been challenged by research showing that some screenings can lead to overdiagnosis and unnecessary treatments that may cause more harm than benefit. The belief that supplements can replace a healthy diet has been debunked by research consistently showing that whole foods provide synergistic benefits that cannot be replicated by isolated nutrients in pill form. The idea that preventive health is expensive and inaccessible has been challenged by research demonstrating that many of the most effective preventive measures such as regular physical activity, healthy eating, and stress management are low-cost or free interventions that provide substantial health benefits.
Core Preventive Health Strategies
Effective preventive health requires a comprehensive approach that addresses multiple aspects of lifestyle, environment, and healthcare utilization to maximize protection against disease while enhancing overall well-being.
Nutrition and Lifestyle Medicine
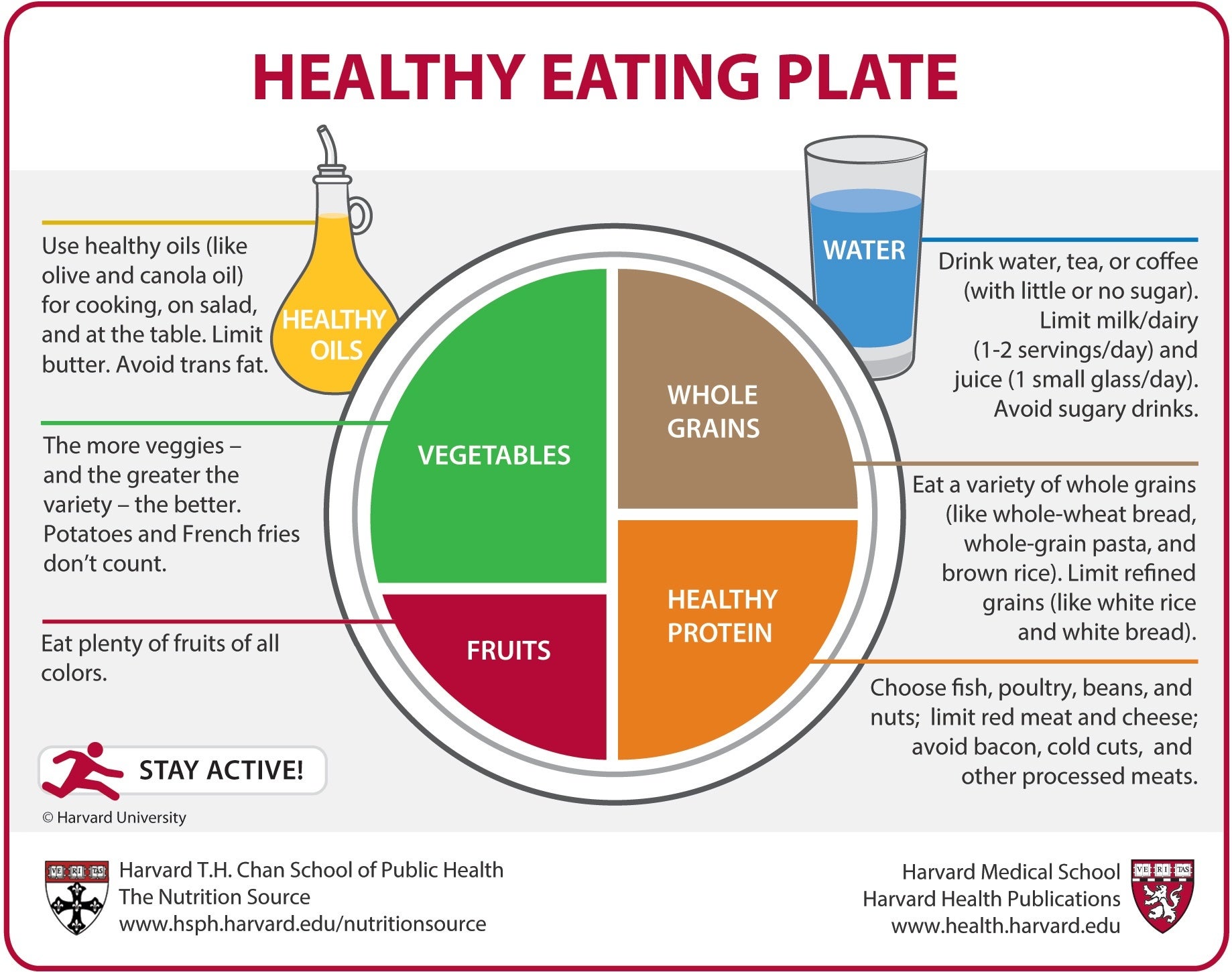
Nutrition forms the foundation of preventive health, with research consistently showing that dietary patterns significantly influence the risk of chronic diseases including cardiovascular disease, diabetes, cancer, and neurodegenerative conditions. The Mediterranean diet, characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil with moderate fish and poultry consumption, has been extensively studied and shown to reduce the risk of cardiovascular disease, cognitive decline, and overall mortality. Plant-based dietary patterns emphasizing whole foods while minimizing processed foods, added sugars, and excessive sodium have been associated with lower rates of chronic diseases and improved health outcomes. Lifestyle medicine approaches integrate nutrition with other evidence-based interventions including regular physical activity, stress management, adequate sleep, and avoidance of harmful substances to address the root causes of disease. The concept of food as medicine recognizes that dietary choices can have therapeutic effects comparable to or exceeding those of conventional medical treatments for many chronic conditions.
Physical Activity and Movement
Regular physical activity is one of the most powerful preventive health interventions, with research consistently showing benefits across virtually all aspects of health including cardiovascular disease prevention, diabetes management, cancer risk reduction, and mental health improvement. The World Health Organization recommends at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days per week for substantial health benefits. Exercise prescription should be individualized based on current fitness level, health status, and personal preferences to ensure safety and adherence while maximizing benefits. Sedentary behavior reduction is increasingly recognized as an important component of preventive health, with research showing that prolonged sitting increases disease risk independent of exercise levels. Environmental and social factors that support physical activity including walkable neighborhoods, access to recreational facilities, and social support for active lifestyles play crucial roles in maintaining long-term adherence to exercise programs.
Healthcare Utilization and Screening
Effective preventive health requires appropriate utilization of healthcare services including evidence-based screenings, vaccinations, and preventive interventions that can detect and address health issues before they become serious problems.
Evidence-Based Screening Guidelines
Medical screening recommendations are based on rigorous evaluation of benefits, harms, and cost-effectiveness to ensure that screening programs provide net health benefits for specific populations. Cancer screening guidelines vary by type of cancer, age, sex, and individual risk factors, with regular mammography, cervical cancer screening, and colorectal cancer screening shown to reduce mortality when appropriately applied. Cardiovascular disease screening includes blood pressure monitoring, cholesterol testing, and diabetes screening that can identify individuals at risk for heart attack, stroke, and other cardiovascular events. Bone density screening for osteoporosis is recommended for women over 65 and men over 70, or earlier for individuals with risk factors such as family history or long-term steroid use. Vision and hearing screening become increasingly important with age, as early detection and correction of sensory impairments can prevent falls, social isolation, and cognitive decline.
Vaccination and Immunization
Vaccination represents one of the most successful preventive health interventions in human history, having virtually eliminated diseases such as polio and significantly reduced the incidence of measles, pertussis, and other infectious diseases. Adult immunization schedules include annual influenza vaccination, pneumococcal vaccines for older adults and those with chronic conditions, and tetanus-diphtheria-pertussis boosters every 10 years. Travel vaccines and preventive medications may be necessary for individuals traveling to areas with specific health risks, requiring consultation with healthcare providers or travel medicine specialists. Herd immunity protects vulnerable populations who cannot be vaccinated due to medical conditions, emphasizing the community benefit of widespread vaccination programs. Staying current with recommended vaccines throughout the lifespan ensures continued protection against preventable diseases while reducing healthcare costs and disease burden.
Environmental and Social Determinants
Preventive health extends beyond individual behaviors to encompass environmental and social factors that significantly influence health outcomes and require community-level interventions for optimal effectiveness.
Environmental Health Factors
Air quality significantly impacts respiratory and cardiovascular health, with research showing that exposure to air pollution increases the risk of asthma, lung cancer, heart disease, and stroke. Water quality and safety are fundamental to health, with access to clean drinking water preventing waterborne diseases and supporting overall well-being. Housing conditions including mold, lead exposure, and overcrowding can significantly impact health outcomes, particularly for children and vulnerable populations. Climate change poses emerging health risks including heat-related illness, vector-borne diseases, and mental health impacts that require adaptive preventive strategies. Reducing exposure to environmental toxins including pesticides, industrial chemicals, and endocrine disruptors can help prevent chronic diseases and support long-term health.
Social Determinants of Health
Social determinants including income, education, employment, housing stability, and social support have profound impacts on health outcomes that often exceed the influence of individual health behaviors or medical care. Food security and access to nutritious foods are fundamental to preventive health, with food insecurity associated with higher rates of chronic diseases and poorer health outcomes. Educational attainment strongly correlates with health literacy, healthcare access, and adoption of preventive health behaviors that support long-term well-being. Employment conditions including job security, workplace safety, and work-life balance significantly influence stress levels and health behaviors that impact preventive health outcomes. Social connections and community engagement provide emotional support, practical assistance, and motivation for maintaining healthy behaviors while buffering against stress and mental health challenges.
Conclusion
Preventive health care provides a solid foundation for maintaining long-term well-being and reducing the risk of chronic diseases that account for the majority of healthcare costs and personal suffering in modern society. By understanding the fundamental principles of disease prevention, implementing evidence-based lifestyle strategies, and appropriately utilizing healthcare services, individuals can take proactive control of their health outcomes while potentially avoiding the physical, emotional, and financial costs associated with chronic disease management. The key to successful preventive health lies in recognizing that it is a comprehensive approach that encompasses nutrition, physical activity, stress management, environmental factors, and appropriate medical care rather than a single intervention or quick fix. Effective preventive health also requires understanding that small, consistent changes are more sustainable and effective than dramatic overhauls that are difficult to maintain over time. By approaching preventive health as an ongoing practice rather than a destination, individuals can develop the knowledge and habits necessary to support optimal health throughout their lives. Remember that preventive health is an investment in future well-being that pays dividends through improved quality of life, reduced healthcare costs, and increased longevity. With education, planning, and consistent implementation, anyone can develop the preventive health strategies necessary to achieve lasting wellness and disease prevention.